Prostatitis is a common urinary disorder that can occur in any man over the age of 30, and the likelihood of its development increases every year. The disease can cause serious problems in men: acute prostatitis can cause depression, decreased libido, and often disrupts the genitourinary system; chronic disease can cause urinary problems, infertility, impotence.
General information
Prostatitis is an inflammatory disease of the prostate, an organ that is only found in men. Iron executive three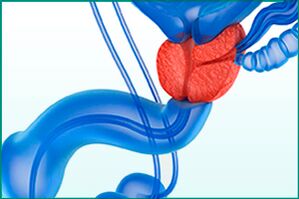 Most important features:
Most important features:
- Secretion - produces a special enzyme that regulates the viscosity of sperm and ensures the viability of male reproductive cells, allowing the successful fertilization of an egg;
- exercise - the musculature that controls the urethral sphincter so that the correct flow of urine occurs and the secretions of the prostate are released during ejaculation;
- Barrier - Prevents infectious agents from entering the upper urinary tract from the urethra, provides an antimicrobial barrier as part of the male immune system.
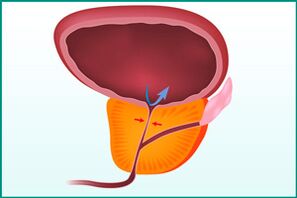
With prostatitis, the prostate enlarges and begins to squeeze the urethra, disrupting the normal flow of urine. Due to inflammation, the organ itself cannot perform its full function.
reason
The root cause of men's health problems - prostatitis - can develop due to:
- Congestion is present in the pelvic region. Most of the time, this bruising occurs due to a sedentary lifestyle and being overweight.
- Prostate infection. It can descend (through the urine) or rise (through the urethra) to enter the prostate with blood or lymph.
The development of prostatitis usually occurs in the context of the presence of certain risk factors:
- lack of physical activity;
- maintain a sedentary lifestyle;
- irregular sex life;
- hypothermia, especially covering the small pelvis;
- Whether there is damage to the pelvic area;
- decrease in immunity;
- Malnutrition rich in sweets, fats and fried foods;
- the presence of bad habits;
- Infectious sexually transmitted infections.
type
According to ICD-10 (International Classification of Diseases), prostatitis is classified into 4 types:
- Acute prostatitis.
- Chronic bacterial prostatitis.
- Chronic prostatitis is non-bacterial, inflammatory and non-inflammatory.
- Chronic prostatitis, asymptomatic.
In the acute form of the disease, the symptoms appear intense and clear, and the inflammatory process develops rapidly. A common cause is infection of the prostate by infectious agents penetrating from the urethra or blood.
Chronic bacterial form - acute prostatitis, which is not cured in time. The same factors that influence acute inflammation contribute to the development of pathological conditions - urogenital infections and blood stasis in the pelvic organs.
Nonbacterial chronic prostatitis (also called chronic pelvic pain syndrome) is most common in older men. It can develop both in the context of impaired prostate function and as a result of the body's autoimmune response.
Chronic asymptomatic prostatitis is inflammation of the prostate gland during which the patient does not show any unpleasant sensations.
Clinic
The clinical manifestations of acute prostatitis have very distinct manifestations, which cannot be ignored or tolerated:
- an increase in body temperature over 38°C;
- cold sweats and weakness;
- Severe pain in the lower abdomen, perineum, genitals;
- Urinary disturbance - difficulty, soreness, acute urinary retention.
In the case of chronic prostatitis, there are similar but less obvious symptoms that are often overlooked:
- Dull pain in the perineum and lower abdomen, radiating to the sacrum and genitals;
- Difficulty, pain, and rapid urination, accompanied by an urgent (sharp and irresistible) urge, most often at night;
- erectile dysfunction;
- Decreased quality and duration of sexual intercourse;
- The severity of the orgasm is reduced.
The asymptomatic course of prostatitis continued without the patient complaining. The problem was discovered incidentally during prostate and/or urine tests.
diagnosis method
If prostatitis is suspected, a doctor will make a diagnosis, and the first step is to clarify the complaint and study the medical history. Gather information on all symptoms and their development. Follow-up activities are as follows:

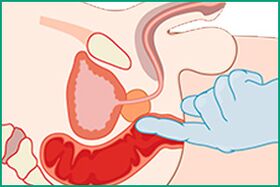
- Palpate the prostate through the rectum to determine the size, density, and pain of the organ. Secrets of the glands were also collected for further bacteriological analysis during probing. The purpose of the study was to rule out some diagnoses: adenoma or prostate cancer, rectal cancer.
- Ultrasound and TRUS to complement and clarify data obtained during palpation.
- Bacteriological analysis of prostate secretions to detect infection and determine the type of pathogen. Data is needed to select and prescribe antibiotics.
- A blood test to determine PSA (prostate-specific antigen) levels - which can rule out adenomas and adenocarcinomas.
- Biopsy - Examination of a sample of prostate tissue under a microscope to confirm or refute adenomas and cancer.
treat
Modern urology considers three approaches to the treatment of acute prostatitis and exacerbation of chronic disease:
- drug;
- surgical;
- physiotherapy.
Drug exposures include taking penicillins, fluoroquinolones, macrolides, tetracyclines, cephalosporins, or aminoglycoside antibiotics. Specific drugs are prescribed by doctors, depending on the infectious agent that causes inflammation. In addition, patients are prescribed:
- Anti-inflammatory drugs to eliminate fever;
- painkiller;
- Antispasmodics to normalize the flow of urine;
- Alpha blockers can relieve symptoms and restore healthy urination.
In the absence of medication effects or in advanced cases of acute prostatitis, doctors may prescribe surgical intervention, during which the entire prostate or part of the prostate is removed. Surgery is necessary for patients with concomitant problems: prostate stones or benign and malignant tumors.
Physiotherapy is complementary to drug therapy and should only be performed after the acute inflammatory process has resolved. Show patients:
- massage;
- exercise therapy (physiotherapy);
- magnetic therapy;
- ultrasound therapy;
- electrical stimulation;
- microwave and laser irradiation;
- Reflexology.
A specific type of procedure is prescribed by the attending physician.
In chronic prostatitis in remission, the patient needs:
- regular check-ups and, if necessary, antibiotic treatment;
- Eat right to avoid fatigue and excess weight;
- protect the body from hypothermia;
- Exercise therapy, exercise should strengthen the lower abdominal and pelvic floor muscles;
- regular sex life;
- Get rid of bad habits.
Another useful procedure is prostate massage, as it improves blood circulation and secretion flow in the organ, which helps prevent recurrence of the acute phase of the disease.
complication
Complications of prostatitis manifest in the prostate itself and in the organs surrounding it, due to its anatomical location. In the acute form, infectious agents are able to reach the bladder and kidneys, inflammation - to the fatty tissue of the glands, venous plexus and rectum.
Chronic disease is dangerous because it involves not only the tissues and organs around the prostate, but also the nerves, urinary and reproductive areas.
Possible complications of acute prostatitis:
- abscess;
- Phlebitis of the small pelvic venous plexus;
- Inflammation of adipose tissue;
- orchitis;
- epididymitis;
- seminal vesiculitis;
- Pyelonephritis.
Chronic prostatitis can lead to the following complications:
- chronic pain syndrome;
- sexual dysfunction;
- infertility;
- Violation of the urination process;
- Quality of life generally declines.
Impotence and Infertility
The two most common problems associated with prostatitis are impotence and infertility. The development of each condition occurs against the background of chronic damage to the prostate.
Impotence (erectile dysfunction) manifests in 40% of neglected and untreated cases of prostatitis. Complications develop over a long period of time, sometimes for years. His reason:
- Nerve impulses invade the prostate through wrong channels and hormone production failure;
- Deterioration of control of the pelvic muscles that lead to erections;
- psychological uncertainty;
- Pain syndrome, which causes fear of possible failure in bed.
It is impossible to talk about the unconditional link between prostatitis and infertility. The disease has indirect effects on male fertility and only has an advanced chronic course. Causes of fertility problems in the context of prostate damage:
- decreased semen quality;
- Decreased numbers and sperm motility;
- Whether germ cells are damaged or defective;
- Scarring of the vas deferens;
- Secretory function failure;
- Testicular dysfunction.
In acute prostatitis, sperm are damaged, their quality and mobility deteriorate, their formation is defective, and a lower number of male germ cells are produced.
prevention
Prostatitis can be prevented, but it is necessary to constantly follow some prevention recommendations:
- Live a healthy lifestyle, with proper nutrition, reasonable physical and sexual activity, and no bad habits;
- Perform physical therapy exercises aimed at decongesting pelvic organs and strengthening pelvic muscles;
- Get timely examinations by urologists and andrologists;
- Beware of hypothermia.
Prostatitis is a serious disease of the urinary system that can cause significant damage to the male body. It is very important to pay attention to the first signs of its appearance and visit a specialist who will prescribe comprehensive treatment. Without this, acute illnesses can become chronic and lead to larger health problems.























