causes of inflammation
- Hypothermia, one-time or related to the nature of outdoor work.
- A sedentary lifestyle can lead to digestive system disorders.
- Chronic physical diseases (diabetes, hypertension).
- Lesion and peri-lesion infection (rhinitis, tonsillitis, stomatitis, gastritis).
- Persistent UGI (chlamydia, trichomoniasis, herpes viruses).
- Stress, insomnia, chronic fatigue syndrome.
- Decreased immunity due to illness, surgery, emotional stress.
- Bad habits that lead to poisoning: alcohol, smoking, strong coffee.
- Occupational injuries to the perineum of car drivers, athletes, and workers in hazardous industries.
- Disturbed sexual intercourse, interruption of intercourse, lack of intercourse, incomplete ejaculation, chronic lack of intimacy (low demand for sperm leading to glandular stagnation).
- STDs.
symptoms of prostatitis
- Discomfort during urination, uncontrolled urination;
- Efficacy impairment, weak erections, decreased libido;
- Difficulty urinating, feeling like your bladder is not completely emptying;
- Perineal pain when sitting for long periods of time, such as while driving;
- Infertility.
- Frequent painful urge to urinate;
- Delayed urination or inability to urinate;
- Throbbing pain in the perineum that passes to the anus and worsens with defecation. As a result, bowel movements become difficult;
- The body is generally in a state of poisoning and fever.
- slight increase in body temperature;
- persistent fatigue;
- Mild pain in the perineum and burning sensation in the urethra;
- Discomfort during urination and defecation;
- Reduced sexual function and resulting psychological depression.
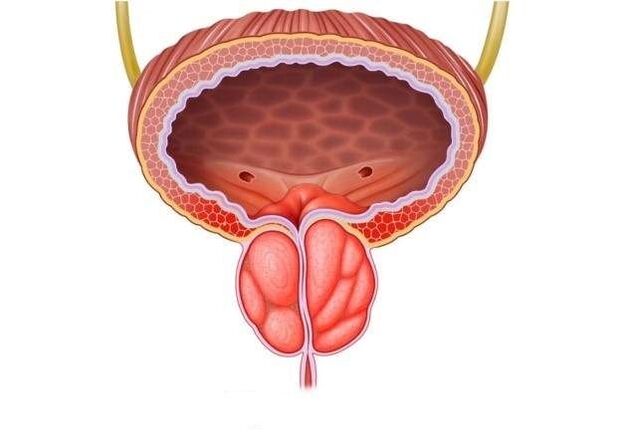
Classification
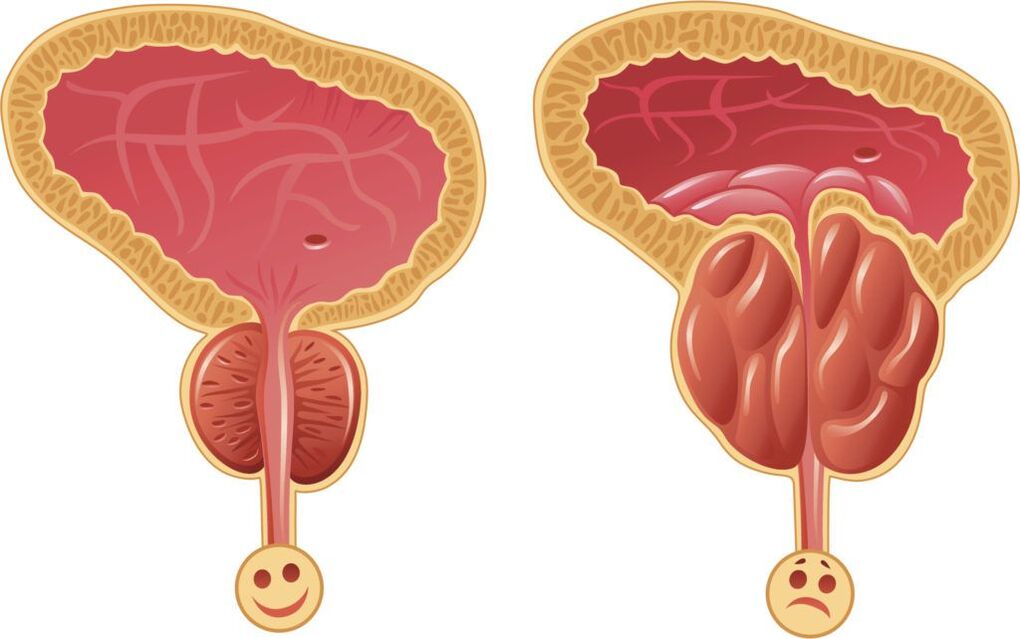
- Acute prostatitis. It affects more than 50% of people aged 30 to 35 years and younger.
- Chronic choice. It is considered a non-age category. It does not manifest itself over a long period of time; the impetus for its development is a cold or infection.
- Bacterial inflammation of the prostate occurs mainly in men under 40 years of age, occurs on the background of ultrasonography, and does not extend beyond the borders of the organ.
- Non-bacterial pathological changes of the glands are mainly chronic.
- Viral inflammation of the prostate is characterized by an acute course affecting the entire genital region.
- Fibrous prostatitis is characterized by rapid and irreversible growth of the gland and requires radical intervention. Clinically resembles prostate adenoma.
- Prostatolithic inflammation occurs due to the formation of stones within the prostate. Considered a precursor to cancer.
- Congestive prostatitis is a result of a sedentary lifestyle and one in every two patients is diagnosed with it.
signs of disease
- Urination disorder, characterized by an intermittent, weak, and abnormally short flow of urine that causes splashing, difficulty, and pain before urinating. Frequent urges to empty your bladder occur mostly at night.
- The pain is localized in the lower abdomen and radiates to the scrotum, perineum, and rectum.
- Sexual dysfunction.
- Ejaculation problems, sperm changes (consistency, quantity).
acute prostatitis
- Seminal vesiculitis is inflammation of the seminal vesicles and is responsible for the presence of pus in sperm, which not only reduces the quality of ejaculation but also leads to loss of reproductive function.
- Colonitis - inflammatory changes in the spermatozoa become the cause of severe pain during sexual intercourse, interrupted orgasm and psychogenic impotence.
- The formation and rupture of abscesses in the prostate and purulent lesions of the rectum can lead to worsening of symptoms, severe physical intoxication, and even death.
- Stagnation of prostate tissue causes changes in its structure, disrupting the innervation and blood supply of the gland itself and nearby organs, thereby disrupting its function. Erection is insufficient for adequate sexual intercourse, premature ejaculation and prolonged intercourse without orgasm are observed.
- Scarring changes to the glands and spermatic cord can lead to infertility, decreased sperm quality and sperm motility. Narrowing of the urethra can interfere with the normal urination process; bladder obstruction can lead to acute urinary retention, requiring emergency surgery.
chronic prostatitis
- fever;
- Pain occurs in the scrotum, perineum, anus, and back;
- Urination disorders;
- Mucus or mucopurulent discharge from the rectum or urethra even without urination or defecation;
- Erectile dysfunction, painful ejaculation, interrupted intercourse, prolonged intercourse without satisfaction.
- Infertility is the result of chronic inflammation of the spermatic cord, vesicles, testicles and their appendages.
- Cystitis, pyelonephritis (other diseases of the genitourinary system) are the result of hematogenous and mechanical spread of microorganisms.
- septicemia.
- Immunity continues to decline.
- Untreated prostatitis can lead to cancer in 35-40% of cases.
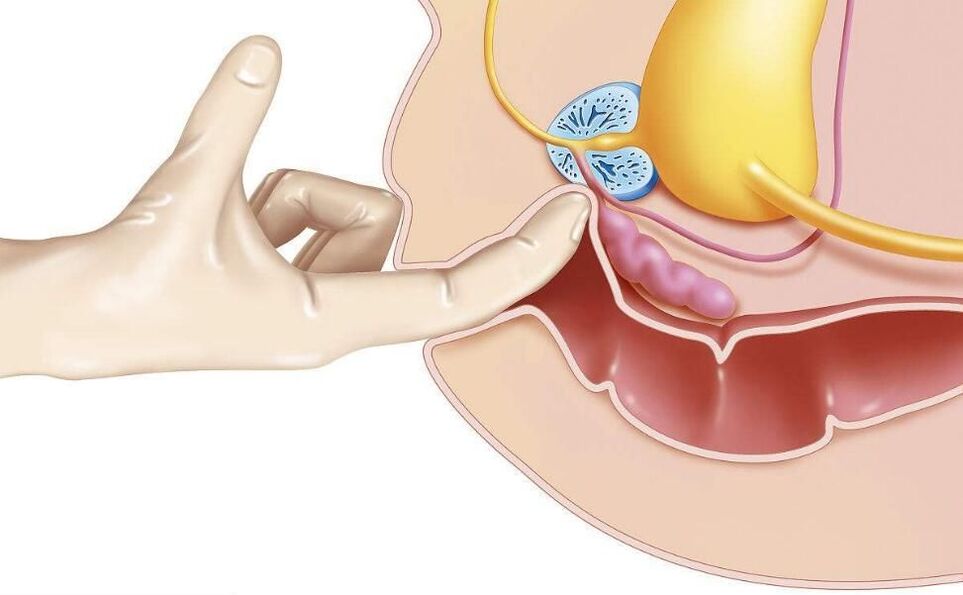
diagnosis
- Glandular rectal examination, aspiration of secretions for examination (culture to determine susceptibility to antibiotics).
- UAC, UAM, urine bacterial culture.
- STD smear test, upper gastrointestinal tract examination.
- The urinary rhythm is monitored daily and the urinary rate is measured (uroflowmetry).
- Perform ultrasound or TRUS for differential diagnosis.
- If tumor needs to be ruled out, a biopsy, urogram, and PSA (prostate-specific antigen) determination are performed.
- To diagnose infertility, a sperm test is performed - the analysis of semen to determine a man's fertility.

Treatment of acute prostatitis
- The most effective treatment for prostatitis is allotropic therapy. If the basis of prostatitis is infection, a course of antibacterial drugs is preferred to relieve the manifestations of inflammation.
- Pain syndromes can be relieved with analgesics, antispasmodics, rectal suppositories, microenemas containing warm analgesic solutions. Nonsteroidal anti-inflammatory drugs may be used.
- Combinations of immunostimulants, immunomodulators, enzymes, vitamin complexes and trace elements have proven their effectiveness.
- Physiotherapy methods are possible only in the subacute stage of the disease. They improve microcirculation and increase immunity: UHF, microwave, electrophoresis, laser, magnetic therapy.
- Massage is another effective way to affect the prostate. It opens the ducts and normalizes blood circulation in the scrotum and pelvis.
- Acute renal filtrate retention can be corrected with catheterization and trocar cystostomy.
- The purulent process involves surgical intervention.
- Consultation with a psychologist.
- antibiotic.Use drugs with broad-spectrum activity that are bactericidal against most pathogens. In most cases, antimicrobial therapy is an allotropic measure, since in most cases the cause of prostatic inflammation is microbial pathogens. For bacterial infections, antibiotics are prescribed, for viral infections, antiviral drugs, and if protozoa are detected, antitrichomoniasis drugs are prescribed. The selection of antimicrobial agents is made empirically or based on the results of PCR, bacterial microscopy, and bacterial culture. The selection of antimicrobial agents, determination of dosage, frequency and duration of administration can be left entirely to the attending physician. In addition to antibiotics, urinary tract disinfectants can be used, which have a disinfecting effect on the mucosa of the genitourinary tract.
- anti-inflammatory drugs.The severity of tissue swelling and the intensity of pain can be reduced. Usually, nonsteroidal anti-inflammatory drugs (NSAIDs) are used.
- Vascular Drugs– Reduces tissue swelling and decongests the prostate, thereby helping to reduce pain and improve blood circulation and local metabolic processes in the tissue.
- enzyme– Dilutes prostate secretions and promotes drainage of pus. In addition, enzymatic drugs increase the effectiveness of antimicrobial therapy by improving the absorption of their active substances into the affected tissues.
- Diuretics (diuretics).They increase urine output, thereby helping to mechanically "flush" the infection.
- Along with antibiotics, patients take hepatoprotective agents to protect the liver parenchyma from toxic damage and improve its functional status.
- To eliminate and prevent the development of intestinal dysbiosis during antibiotic therapy, patients need to take probiotics.
- After the acute inflammation of the prostate subsides, the patient will receive a course of physical therapy - drug electrophoresis, electroplating, magnetic therapy, laser, mud therapy, etc. This type of surgery can improve local microcirculation and lymphatic drainage, metabolic processes and tissue nutrition, stimulate tissue repair, accelerate the final resolution of the inflammatory process, and promote tissue recovery and normalization of prostate functional status.
Treatment of chronic prostatitis
- Herbal preparations are widely used in urological practice. They are able to accumulate at the sites of the most active pathological processes, protect cells from oxidation, scavenge free radicals and prevent glandular tissue proliferation.
- Antimicrobial treatment is selected individually based on the susceptibility of the microorganism to the drug.
- Immunity-boosting medications not only help deal with prostatitis but can also correct the negative effects of antibiotics that disrupt immune system function.
- Pain syndrome can be relieved by taking alpha-blockers and muscle relaxants.
- Prostate massage can mechanically remove "excess" secretions from the gland through the urethra, improve circulation, and minimize congestion.
- Physical therapy: laser, magnet, ultrasound, iontophoresis, warm sitz bath or herbal micro-enema.
- In severe cases, intravenous fluids containing diuretics may be needed. This stimulates the production of large amounts of urine, preventing the development of symptoms of intoxication, ascending cystitis, and pyelonephritis.
- For constipation, herbal laxatives can be used.
- Urologists and psychologists work with patients to develop a personal long-term plan that includes daily living, necessary rest, diet, moderate physical activity, and sexual activity.
- If the chronic process is resistant to treatment and the outflow of urine is blocked, surgical intervention is required: removal of all affected tissue (transurethral resection of the prostate) or complete removal of the gland and its surrounding tissue (prostatectomy). Practiced under special circumstances, it can lead to impotence and urinary incontinence. Young people do not undergo surgery because it can lead to infertility.
medical treatement
antibacterial treatment
physiotherapy
- magnet therapy;
- Laser Treatment;
- electrophoresis;
- warm up;
- ultrasound;
- mud therapy;
- high frequency irradiation;
- physiotherapy.
non-specific treatment
- leech therapy;
- therapeutic fasting;
- acupuncture;
- Diet according to the Ostrovsky method;
- Alkalize the body using the Neumyvakin method.
Surgery
- For the drainage of purulent abscesses, which can be removed by puncture via laparoscopic approach;
- Difficulty urinating due to damage to the urinary tract;
- The affected area is large;
- There are numerous stones in the gland.
folk remedies

prostatitis suppositories
- Antibacterial agents are particularly effective against prostatitis caused by chlamydia.
- Painkillers are used for symptomatic treatment; they provide good pain relief.
- Immunostimulants help improve circulation, relieve swelling, and are used in complex treatments.
- Herbs have a mild effect. They are like candles on bee products and are used as a supplement to primary treatments.
- Ichthyol-based compositions promote blood flow in the intestinal mucosal area, thereby accelerating the attenuation of inflammatory processes and slightly improving immunity.
- Products based on special enzymes prevent the formation of scar tissue. It is recommended as part of a combination of antibiotics, anti-inflammatory drugs and analgesics.
auxiliary medicine
diet and lifestyle
Consequences of untreated prostatitis
prevention
- Maintain a healthy lifestyle and quit bad habits.
- Don't be too cold.
- Drink at least 1. 5-2 liters of water daily.
- Strengthen your immune system, walk more, and improve your physical fitness.
- Play sports and visit a health club.
- Avoid stressful situations.
- Maintain a regular sex life with a regular partner.























